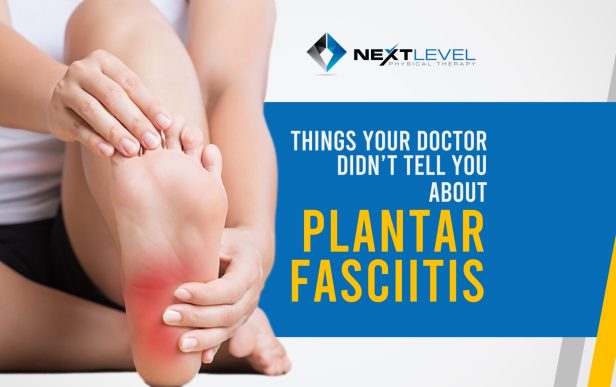
The 3 Things Your Doctor Didn’t Tell You About Plantar Fasiitis
You are reading this because either you, or someone you care about, has been dealing with a persistent burning or aching pain on the bottom of the foot. Maybe it only hurts when walking. Maybe it hurts all the time. Maybe it is in the middle of the arch or closer to the heel.
Either way, chances are a podiatrist or orthopedist has told you that it is plantar fasciitis. Here are three things they probably did not tell you.
There is typically nothing wrong with the foot itself
Typical solutions do not address the root of the problem
Exercise is the only way to truly eliminate it
Let’s get into it.
There is Typically Nothing Wrong With the Foot Itself
Plantar fasciitis is classified as an inflammatory condition, but inflammation itself is not the problem. Inflammation often gets a bad reputation, but it is actually a critical part of the healing process.
When tissue damage occurs, even at a mild level, inflammation shows up to start repair. Think of a car accident on the highway where a guardrail is damaged. Police arrive to secure the area, tow trucks remove vehicles, street cleaners clear debris, and construction crews rebuild the rail. Inflammation serves a similar purpose in the body. It clears debris and delivers materials needed for healing.
Inflammation only becomes an issue when it never resolves. If inflammation represents the first step in healing, then chronic inflammation means the body is constantly trying to repair damage but never catching up. This is the definition of an overuse injury.
With plantar fasciitis specifically, the pain in the foot is usually the result of a problem, not the problem itself. Flat feet, high arches, or family history are rarely the primary cause. If the structure of your foot were the issue, pain would have shown up much earlier in life.
Typical Solutions Don’t Address the Root of the Problem
Common treatments include rest, boots, stretching, massage, cortisone injections, and orthotics. While these can help reduce pain, they often miss the bigger picture when used alone.
The goal of early treatment is to reduce stress on the plantar fascia so healing can occur. A boot, night splint, or rest period lowers overall load. Pain decreases and things feel better for a while. Then the boot comes off, life returns to normal, and weeks later the pain slowly creeps back in.
That is not bad luck. The strain did not happen randomly.
You felt better because support and reduced activity offloaded stress. Once normal movement and load returned, the same stresses were placed on the same tissues.
Stretching and massage often follow next. Rolling the foot on a frozen water bottle and stretching the calves can feel great temporarily. Relief lasts an hour, then symptoms return, so the cycle repeats. Temporary relief is mistaken for progress.
Cortisone injections often come next. They can dramatically reduce pain by suppressing inflammation. The problem is that inflammation is not the root issue. Removing the warning signal does not eliminate the stress causing the problem.
All of these approaches treat symptoms, not causes. They can create a window of opportunity to do the real work, but they are rarely sufficient on their own.
Exercise is the Only Way to Truly Eliminate It
If most treatments focus on reducing pain, then exercise must address why the pain exists in the first place.
That usually means strengthening the foot and improving how forces move through the body.
Strengthening is straightforward. Strong tissues tolerate more stress before breaking down. This allows you to do more without accumulating overuse. Unfortunately, seated calf raises and toe curls only take you so far.
To truly change capacity, exercises like walking, farmer carries, step ups, step downs, split squats, lunges, and light plyometrics must be part of the plan.
The other major factor is motor variance. For this discussion, motor variance means how many movement options you can access and control. The more positions your foot, ankle, and lower leg can move through, the less wear any single tissue experiences.
Think of it like shoes. If you wore the same pair every day, they would break down quickly. Rotating through several pairs spreads the stress.
Stretching and massage temporarily improve range of motion, but range of motion is driven by muscle activity. If stiffness keeps returning, those muscles are doing a job. The key is figuring out why.
That often means looking above the foot.
What if plantar fasciitis pain is influenced by your upper back? The position of your center of mass has a major impact on your feet. If the upper back, lower back, or hips are stiff, they can push your body weight forward. As your weight shifts forward, your calves and feet must work harder to keep you upright.
You push your toes into the ground to prevent falling forward, which increases stress through the plantar fascia, calves, and Achilles. Muscles tighten to protect you from tipping. Suddenly foot pain is not just a foot problem.
This is why any approach to plantar fasciitis that ignores center of mass is incomplete.
If you have been dealing with foot pain for a long time and nothing seems to work, widen your lens. Do not stare at one tree so closely that you miss the forest.
Read More